The testicles (also called testes) are part of the male reproductive system. The testicles are two oval organs about the size of large olives. They are located inside the scrotum, the loose sac of skin that hangs behind the penis. The testicles make the male hormones, including testosterone, and produce sperm, the male reproductive cells. Disorders of the testes can lead to serious complications, including hormonal imbalances, sexual dysfunction, and infertility.
What disorders affect the testes?
Some of the more common disorders that affect the testes include the following:
Testicular trauma
Because the testes are located within the scrotum, which hangs outside of the body, they do not have the protection of muscles and bones. This makes it easier for the testes to be struck, hit, kicked or crushed, which occurs most often during contact sports. Males can protect their testicles by wearing athletic cups during sports.
Trauma to the testes can cause severe pain, bruising and/or swelling. In most cases, the testes—which are made of a spongy material—can absorb the shock of an injury without serious damage. A rare type of testicular trauma, called testicular rupture, occurs when the testicle receives a direct blow or is squeezed against the hard surface of the pelvis. This injury can cause blood to leak into the scrotum. In severe cases, surgery to repair the rupture—and thus save the testicle—may be necessary.
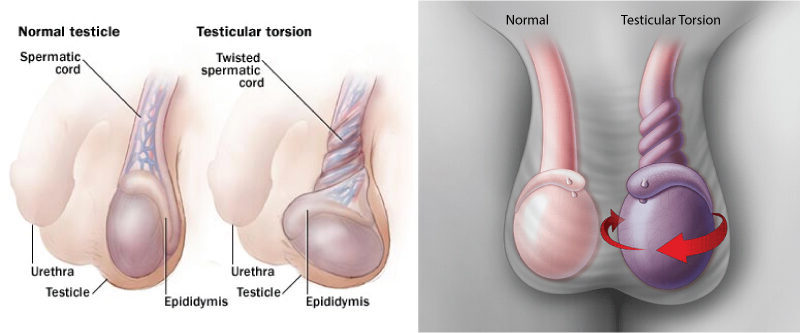
Testicular torsion
Within the scrotum, the testicles are secured at one end by a structure called the spermatic cord. Sometimes, this cord gets twisted cutting off the testicle’s blood supply. Symptoms of testicular torsion include sudden and severe pain, enlargement of the affected testicle, tenderness, and swelling.
This disorder, which occurs most often in young males between the ages of 12 and 18, can result from an injury to the testicles or strenuous activity. It also can occur for no apparent reason.
Testicular torsion is an emergency. Treatment usually involves correction of the problem through surgery. The testicular function may be saved if the condition is diagnosed and corrected immediately. If the blood supply to the testicle is cut off for a long period, the testicle can become permanently damaged and may need to be removed.
Testicular cancer
Testicular cancer occurs when abnormal cells in the testicles divide and grow uncontrolled. Testicular cancer can develop in one or both testicles in men or young boys. Symptoms of testicular cancer include a lump, irregularity or enlargement in either testicle; a pulling sensation or feeling of unusual heaviness in the scrotum; a dull ache in the groin or lower abdomen; and pain or discomfort (which may come and go) in a testicle or the scrotum.
The exact causes of testicular cancer are not known, but there are certain risk factors for the disease. A risk factor is anything that increases a person’s chance of getting a disease. The risk factors for cancer of the testicles include:
- Age — Testicular cancer can occur at any age, but most often occurs in men between the ages of 15 and 40.
- Undescended testicle (cryptorchidism) — This is a condition in which the testicles do not descend from the abdomen, where they are located during development, to the scrotum shortly before birth. This condition is a major risk factor for testicular cancer.
- Family history — A family history of testicular cancer increases the risk.
- Race and ethnicity — The risk for testicular cancer in Caucasian men is more than five times that of African-American men and more than double that of Asian-American men.
Testicular cancer is a rare form of cancer and is highly treatable and usually curable. Surgery is the most common treatment for testicular cancer. Surgical treatment involves removing the cancerous testicle through an incision (cut) in the groin. In some cases, the doctor also may remove some of the lymph nodes in the abdomen. Radiation, which uses high-energy rays to attack cancer, and chemotherapy, which uses drugs to kill cancer, are other treatment options.
The success of treatment for testicular cancer depends on the stage of the disease when it is first detected and treated. If the cancer is found and treated before it spreads to the lymph nodes, the cure rate is excellent, greater than 98 per cent. Even after testicular cancer has spread to the lymph nodes and other parts of the body, chemotherapy is highly effective, with a cure rate greater than 90 per cent.
To prevent testicular cancer, all men should be familiar with the size and feel of their testicles, so they can detect any changes. The American Cancer Society recommends monthly testicular self-examinations (TSE) for men over age 15. A TSE is best performed after a warm bath or shower when the skin of the scrotum is relaxed. After looking for any changes in appearance, carefully examine each testicle by rolling it between the fingers and thumbs of both hands to check for any lumps.
Epididymitis
Epididymitis is inflammation of the epididymis. The epididymis is the coiled tube that lies on and behind each testicle. It functions in the transport, storage, and maturation of sperm cells that are produced in the testicles. The epididymis connects the testicles with the vas deferens (the tubes that carry sperm).
Epididymitis often is caused by infection or by the sexually transmitted disease chlamydia. Symptoms of epididymitis include scrotal pain and swelling. In severe cases, the infection can spread to the adjacent testicle, causing fever and abscess (collection of pus).
Treatment for epididymitis includes antibiotics (drugs that kill the bacteria causing the infection), bed rest, ice to reduce swelling, the use of a scrotal supporter, and anti-inflammatory medicines (such as ibuprofen). The use of condoms during sex can help prevent epididymitis caused by chlamydia. If left untreated, epididymitis can produce scar tissue, which can block the sperm from leaving the testicle. This can cause problems with fertility, especially if both testicles are involved or if the man has recurring infections.
Hypogonadism
One function of the testes is to secrete the hormone testosterone. This hormone plays an important role in the development and maintenance of many male physical characteristics. These include muscle mass and strength, fat distribution, bone mass, sperm production, and sex drive.
Hypogonadism in men is a disorder that occurs when the testicles (gonads) do not produce enough testosterone. Primary hypogonadism occurs when there is a problem or abnormality in the testicles themselves. Secondary hypogonadism occurs when there is a problem with the pituitary gland in the brain, which sends chemical messages to the testicles to produce testosterone.
Hypogonadism can occur during fetal development, at puberty, or in adult men. When it occurs in adult men, hypogonadism may cause the following problems:
- Erectile dysfunction (the inability to achieve or maintain an erection)
- Infertility
- Decreased sex drive
- The decrease in beard and growth of body hair
- The decrease in size or firmness of the testicles
- The decrease in muscle mass and an increase in body fat
- Enlarged male breast tissue
- Mental and emotional symptoms similar to those of menopause in women (hot flashes, mood swings, irritability, depression, fatigue)
There are various causes of hypogonadism, including:
- Klinefelter’s syndrome — This syndrome involves the presence of abnormal sex chromosomes. A male normally has one X chromosome and one Y chromosome. The Y chromosome contains the genetic material with the codes that determine the male gender, and related masculine characteristics and development. Males with Klinefelter’s syndrome have an extra X chromosome, which causes abnormal development of the testicles.
- Undescended testicles — The testicles develop inside the abdomen and usually move down into the scrotum before birth. Sometimes, this does not occur. However, in most cases, the testicles descend by the child’s first birthday. An undescended testicle that remains outside the scrotum throughout childhood can result in abnormal testicular development.
- Hemochromatosis — Hemochromatosis, or too much iron in the blood, can cause the testicles or the pituitary gland to malfunction.
- Testicular trauma — Damage to the testicles can affect the production of testosterone.
- Cancer treatment — Chemotherapy or radiation therapy, common treatments for cancer, can interfere with testosterone and sperm production by the testicles.
- Normal ageing — Older men generally have lower levels of testosterone, although the decline of the hormone varies greatly among men.
- Pituitary disorders — Problems affecting the pituitary gland—including a head injury or pituitary tumour—can interfere with the gland’s signals to the testicles to produce testosterone.
- Medications — Certain drugs can affect testosterone production. Commonly used psychiatric drugs and some medicines used to treat gastroesophageal reflux disease (GERD) may cause hypogonadism.
Treatment for hypogonadism depends on the cause. Male hormone replacement (testosterone replacement therapy or TRT) often is used to treat disorders of the testicles. If the problem is related to the pituitary gland, pituitary hormones may help increase testosterone levels and sperm production.